Diabetic Foot Management
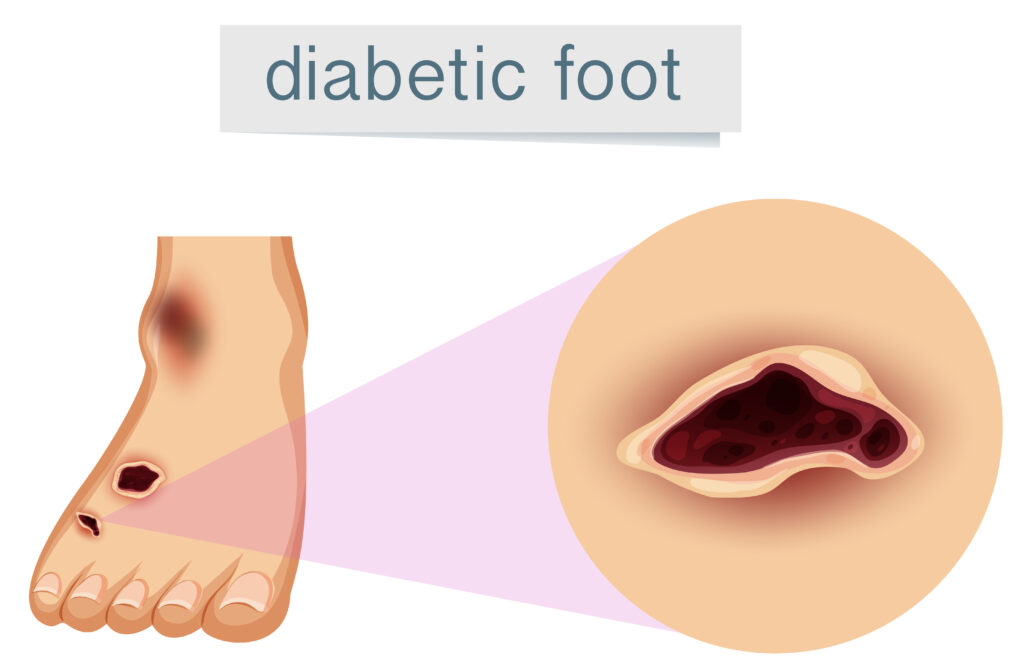
Diabetic foot management refers to the treatment and care of foot problems that arise as a complication of diabetes. People with diabetes are at increased risk of developing foot ulcers, infections, and other complications due to nerve damage (neuropathy) and poor circulation (peripheral arterial disease). Minimally invasive procedures have become an integral part of diabetic foot management, offering less invasive alternatives to traditional surgical techniques.
One common minimally invasive procedure for diabetic foot management is endovascular therapy. Endovascular procedures involve accessing the blood vessels through small incisions or punctures in the skin, typically using catheters and wires guided by imaging techniques such as fluoroscopy or ultrasound. These procedures can be used to improve blood flow to the feet by opening blocked or narrowed arteries, thus promoting wound healing and preventing amputation.
For example, a diabetic patient with peripheral arterial disease may undergo endovascular angioplasty and stenting to widen narrowed arteries in the legs or feet. During angioplasty, a balloon-tipped catheter is inserted into the blocked artery and inflated to compress the plaque buildup and restore blood flow. In some cases, a stent—a small metal mesh tube—is inserted to keep the artery open and prevent re-narrowing.
Another minimally invasive procedure used in diabetic foot management is minimally invasive surgery (MIS) for ulcer debridement and wound closure. MIS techniques involve making small incisions or using specialized instruments to remove infected or dead tissue (debridement) and facilitate wound healing. This approach reduces the risk of complications and promotes faster recovery compared to traditional open surgery.
In addition to endovascular therapy and minimally invasive surgery, other minimally invasive techniques may be utilized in diabetic foot management, including:
Percutaneous decompression: This involves releasing pressure on nerves in the foot using minimally invasive techniques, which can help alleviate pain and prevent further nerve damage in diabetic neuropathy.
Injection therapies: Certain injections, such as platelet-rich plasma (PRP) or growth factors, may be used to promote tissue regeneration and wound healing in diabetic foot ulcers.
Overall, minimally invasive procedures play a crucial role in diabetic foot management by providing effective, less traumatic alternatives to traditional surgery, reducing the risk of complications, and improving outcomes for patients with diabetes.